JOHN ROBERT SILBER
August 15, 1926 - September 27, 2012
A True Champion for Equal Education is Gone...
Left, President Silber poses with BU student Osman Sharrieff Couey at his dormitory security post
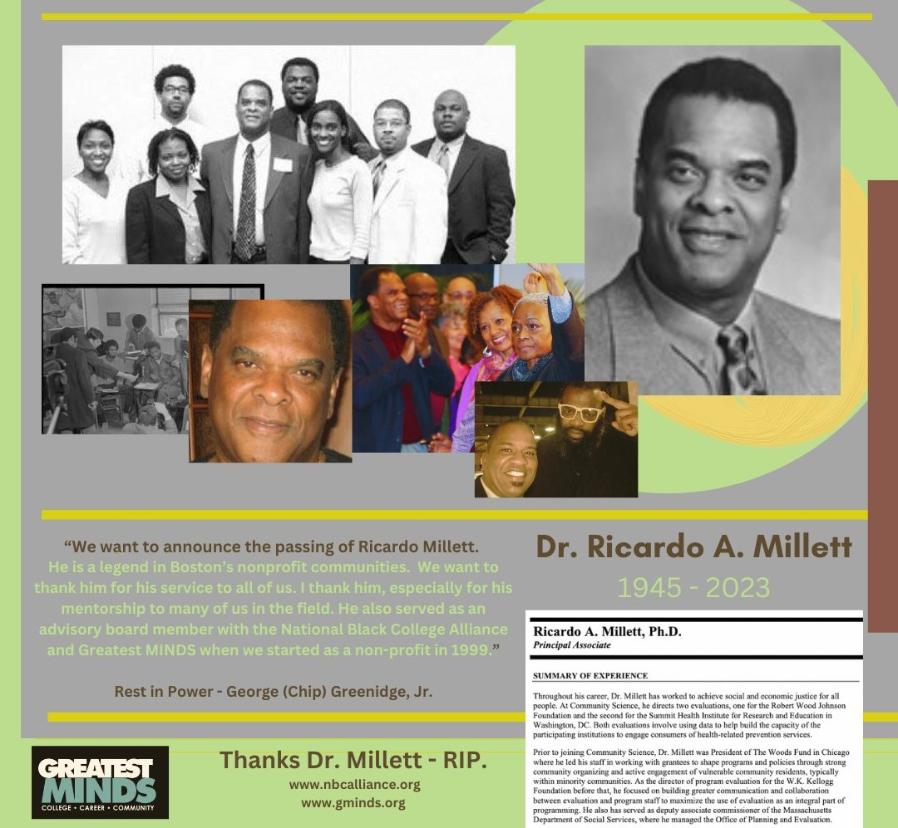
Dr. Ricardo Millett: MLK Center Director
Dr. David French: Pioneering Physician
David French was born and raised in Ohio. Although his father had been forced to withdraw from Howard University as a young man because of lack of money, his parents stressed the importance of education for their own children. He was drafted into the Army during World War II, interrupting his premedical studies to serve in a segregated unit in Texas where he and fellow Black soldiers were assigned to pick cotton for uniforms. He noted that German prisoners of war held in Texas were treated better than Black soldiers seeking to defend our nation. Determined to pursue his dream of becoming a doctor, he enrolled at Howard University School of Medicine through a military program where he was mentored by famed Black surgeon Dr. Charles Drew, who pioneered modern blood banking techniques. David followed in Dr. Drew’s surgical footsteps and went on to establish pediatric cardiovascular surgery departments at Howard, Freedmen’s Hospital, and D.C. General Hospital in Washington, D.C.
As the Civil Rights Movement grew he joined the many unsung heroes—doctors, nurses, and other emergency medical professionals—providing frontline first aid to protesters brutally assaulted during marches. In 1964, few realized the essential service the newly formed Medical Committee for Human Rights performed. Many of the doctors and nurses, including him, took time off from jobs in the North to volunteer in the South. In 1965, David French coordinated the medical volunteers for the voting rights march from Selma to Montgomery, Alabama. After marchers were savagely beaten by state troopers during their first attempt to cross the Edmund Pettus Bridge on “Bloody Sunday,” he saved the day and the lives of the protesters by helping bring in the Johnson White House and the federal troops to protect them in the final march. One year later, as Dr. King, Stokely Carmichael, and other civil rights activists—including myself—completed James Meredith’s march from Memphis to Jackson, Mississippi after Meredith was injured by a sniper, David and Carolyn French joined in using their Dodge Camper as a makeshift ambulance for his medical team.
The Medical Committee’s focus quickly expanded from protecting civil rights workers to fighting inequalities in health care under the motto “Health Care Is a Human Right.” Driven by his passion for social justice, David French shifted his focus from surgery to public health. As he told the Boston Globe, “I became aware of overwhelming health problems in the marches in the deep South, but later realized that urban health problems with regard to delivery of services are just as difficult.’’ He went back to school and earned a masters’ degree in Public Health from Johns Hopkins University. In 1969 he became the first chairman of Boston University’s Department of Community Medicine and was chosen as the first medical director of Roxbury Comprehensive Community Health Center, meeting the needs of one of Boston’s poorest communities. Roxbury Comprehensive Community Health Center was one of the earliest community health centers and became a model for providing health services for the poor.
David French then set his sights on the African continent, believing the community health center model could deliver the crucial primary care so many desperately needed. He and his family of eight beautiful children spent a decade living in the Ivory Coast as he oversaw a program coordinated by the World Health Organization, the U.S. Agency for International Development, the Centers for Disease Control and Prevention, and Boston University that trained health care workers in 20 African countries to set up networks of clinics providing primary and preventive care.
His groundbreaking work helped set the stage for today’s network of community health centers around the world. According to the National Association of Community Health Centers, the United States now has 1,250 community health centers providing vital primary care to 20 million low-income children and adults. This crucial lifeline of services saves between $9.9 billion and $17.6 billion a year by helping patients avoid emergency room care. Last week, the majority of funding for community health centers was saved at the last minute by the compromise budget agreement that averted a government shutdown. How shortsighted, uncaring, and fiscally irresponsible are those who would cut life and cost saving programs. I applaud Vermont Senator Bernie Sanders who has stood up for this vital health safety network through thick and thin. But, community health centers are still at risk in the House budget plan that seeks to dismantle Medicare and Medicaid and balance the budget on the backs of poor children and families. Millions of low-income families are in danger of losing the quality health care they desperately need. Let’s honor the legacy of Dr. David French and the life of urgency he lived and make the right and moral choice to care for America’s poor children and families and preserve—yea expand—the vital network of community health centers.
Marian Wright Edelman is President of the Children's Defense Fund whose Leave No Child Behind® mission is to ensure every child a Healthy Start, a Head Start, a Fair Start, a Safe Start and a Moral Start in life and successful passage to adulthood with the help of caring families and communities. For more information go to www.childrensdefense.org.
David French; healed the sick from Roxbury to Africa
April 06, 2011|By Bryan Marquard, Boston Globe Staff
When Roxbury residents began planning in the mid-1960s to open a groundbreaking clinic, they wanted more than just good doctors.
While creating the first comprehensive health center in the nation that would be under community control, Roxbury residents on a planning committee paid particular attention to the attitude each job candidate had about the clinic and the neighborhood. In Dr. David M. French, they found a skilled physician who had set aside a potentially lucrative career as a pediatric thoracic surgeon to focus on community medicine.
“I became aware of overwhelming health problems in the marches in the deep South,’’ he told the Globe in 1969, “but later realized that urban health problems with regard to delivery of services are just as difficult.’’
Dr. French, the first medical director of the Roxbury Comprehensive Community Health Center and the first chairman of what then was Boston University’s department of community medicine, died of renal failure Thursday in University Hospital in Charlottesville, Va. He was 86 and had been living in Barboursville, Va., in the ancestral home of his late wife.
His career at BU took him in the mid-1970s to Africa, where he ran a 20-country health program launched by institutions and organizations that included the university and the World Health Organization.
For the Roxbury residents, though, Dr. French’s medical and academic credentials made him an appealing candidate. He was fresh from a fellowship at Johns Hopkins University in Baltimore, where he supplemented his medical degree from the College of Medicine at Howard University in Washington, D.C., with a master’s in public health.
He had also directed medical care for historic marches in the civil rights era, including one across Alabama from Selma to Montgomery. His daughter Lynn of Washington, D.C., said that for the James Meredith march from Memphis to Jackson, Miss., in 1966, Dr. French and his wife, Carolyn, used the family van as a de facto ambulance.
In 1969, when Dr. French arrived in Boston, the city was a few years from court-ordered busing to desegregate its public schools. He needed only to read the Globe headline heralding his arrival to know race drew public scrutiny: “Black Doctor to Head Health Center.’’
His jobs at the Roxbury clinic and as a professor at BU straddled the disparate worlds of academia and urban strife.
“A social contract is being established here between the community and a social establishment, Boston University Medical Center,’’ he told the Globe in June 1970. “There is suspicion on both sides.’’
Dr. French was a good choice to allay those fears, for reasons that went beyond his training and social justice background.